Case History: A 15-year-old male presented with a 3-4 month history of persistent left knee pain and swelling. He denied any recent trauma but mentioned a previous incident 3-4 years ago where he struck his knee against a tree branch after climbing it. During his initial evaluation in the emergency department, x-rays revealed a small effusion and a high-riding patella without evidence of acute fractures or dislocations. He denied experiencing mechanical symptoms such as popping, locking, or giving way, and he did not report any systemic symptoms including fever, chills, weight loss, or fatigue. Notably, he had not attempted any structured or formal physical therapy to alleviate his knee pain, nor had he used other therapeutic interventions before this visit.
Physical Examination: Bilateral knees had full active range of motion, although he reported pain and tightness at terminal flexion of left knee due to a large joint effusion. There was tenderness to palpation along the left knee medial and lateral joint lines and peripatellar regions. The patient reported mild discomfort in the left knee with bilateral squats and mild pain with left patellar grind. The right knee was non-tender without effusion. Stability tests, including anterior/posterior drawer, valgus/varus stress, Lachman, McMurray, Apley, Thessaly, dial, and patellar apprehension were all negative. Overall, the examination revealed no mechanical instability or significant joint laxity.
Differential Diagnoses: Lipoma arborescens, juvenile idiopathic arthritis (JIA), pigmented villonodular synovitis (PVNS), synovial chondromatosis, juvenile spondyloarthropathy
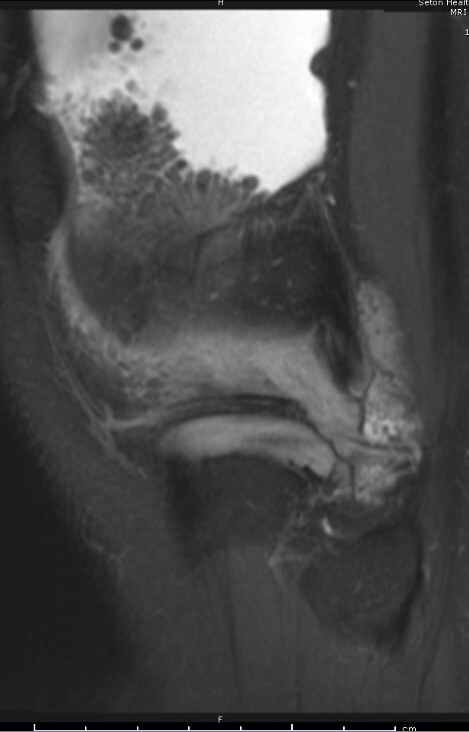
Tests/Results/Imaging: The patient underwent x-ray imaging of the left knee initially, which revealed a small suprapatellar effusion and a high-riding patella with preserved joint spaces and no osseous lesions. An autoimmune work-up (CBC, CMP, ANA, RF, anti-CCP, ESR, CRP) was negative. An MRI of the left knee obtained after the initial workup showed no meniscal tears or ligamentous injuries. Moderate joint fluid was noted with frond-like T1 bright fat hypertrophy throughout indicative of lipoma arborescens.
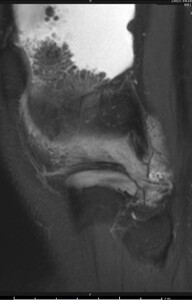
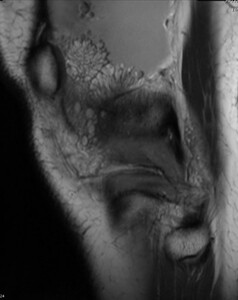
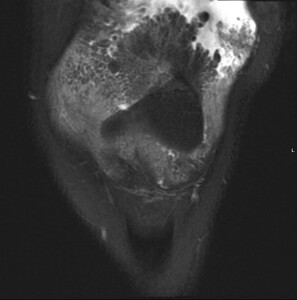
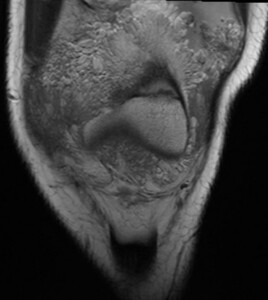
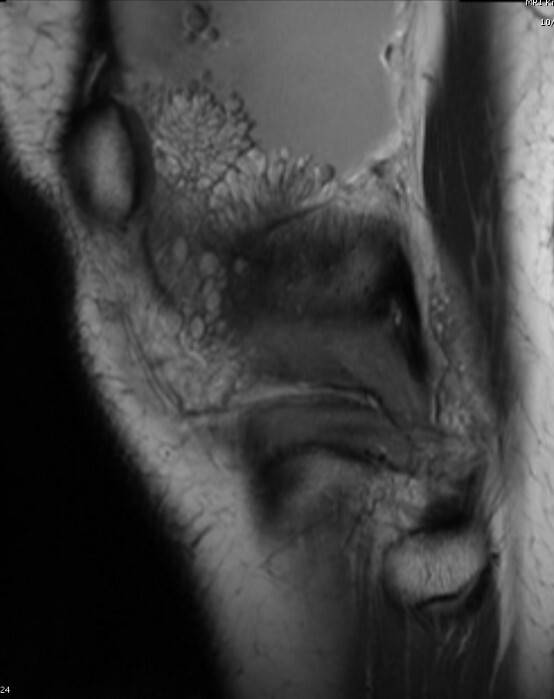
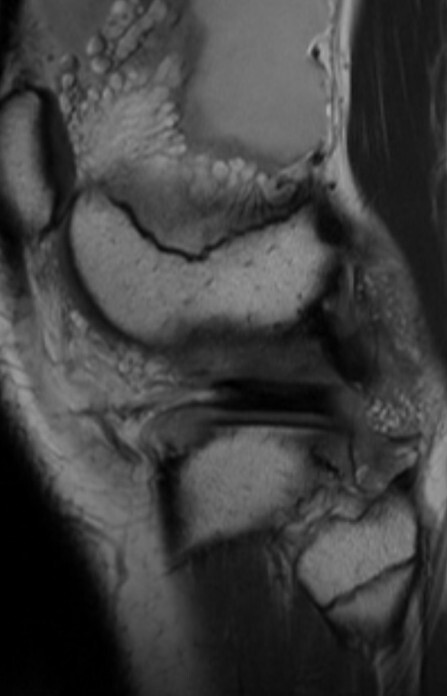
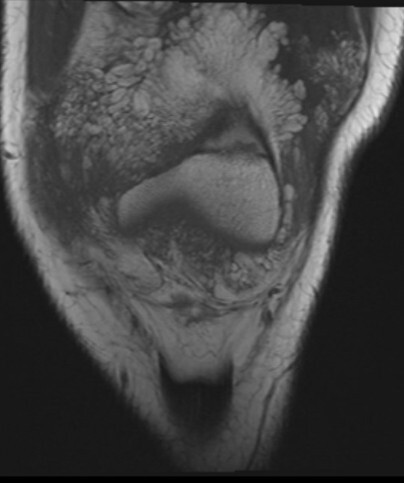
Figure 1 shows a sagittal proton-dense (PD) T2 fat suppression (FS), while Figure 2 indicates a sagittal non-FS T2 with frond-like fat hypertrophy indicative of villous lipomatous proliferation of the synovial membrane.
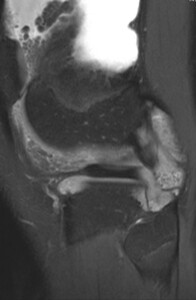
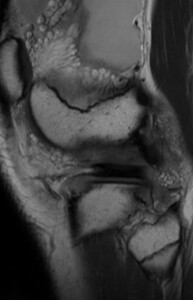
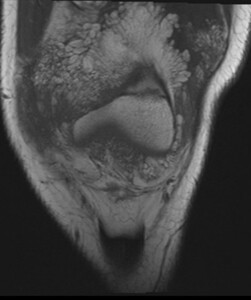
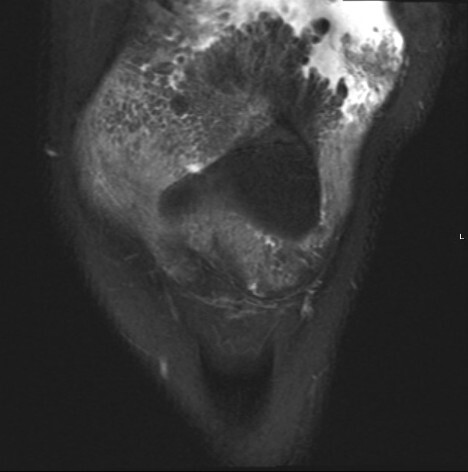
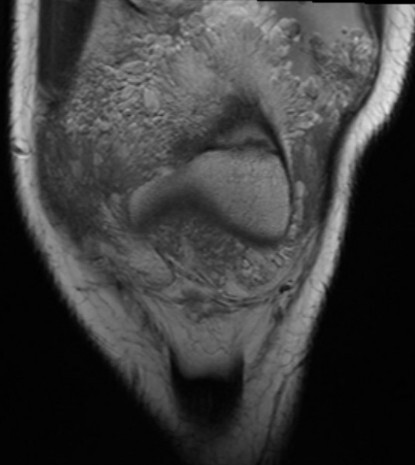
Figure 3 shows a more lateral section of a sagittal proton-dense T2 FS while Figure 4 shows a more lateral section of a sagittal non-FS T2 image indicating the frond-like structures deeper throughout the joint.
Final/Working Diagnosis: Lipoma arborescens
Discussion: Lipoma arborescens is a rare, benign intra-articular lesion marked by chronic knee pain, recurrent effusions, and limited motion, often without prior trauma. It may be primary and idiopathic, typically affecting younger patients, or secondary to chronic synovial irritation from osteoarthritis, trauma, or inflammatory arthropathies. MRI is the diagnostic modality of choice, revealing characteristic frond-like fatty synovial proliferation.
Management ranges from conservative measures—such as NSAIDs, physical therapy, and corticosteroid injections—to surgical synovectomy in cases of persistent symptoms or mechanical impairment. Non-operative treatment may be considered in patients with mild or incidental findings. Surgery is typically reserved for those with recurrent effusions, mechanical symptoms, or functional limitations.
In this case, the patient’s MRI revealed both anterior and posterior disease with ongoing symptoms, and a posterior synovectomy is currently scheduled approximately one year from initial evaluation. Continued monitoring remains essential to assess for underlying inflammatory conditions, particularly in younger patients.
Outcome: Histopathologic examination confirmed the diagnosis following an initial arthroscopic synovectomy. Due to the diffuse nature of the disease, a staged approach was implemented, beginning with minimally invasive resection followed by planned posterior synovectomy.
Postoperatively, the patient was advised to engage in a structured rehabilitation program which emphasized quadriceps strengthening, range of motion exercises, and progressive weight-bearing. Physical therapy was initiated to facilitate functional recovery, and the patient was encouraged to integrate rehabilitation into his school athletics program under supervision.
Return to Activity and Follow-up: A multidisciplinary rehabilitation strategy was employed to optimize functional outcomes and facilitate return to activity. The patient was prescribed formal physical therapy, a structured home exercise program, and use of a compression sleeve, which provided symptomatic relief. At follow-up, improvements in gait mechanics and strength were observed, and further progression of activity was recommended. Given the planned second-stage posterior resection, continued monitoring and phased rehabilitation will be essential, and continued postoperative reassessments will guide a safe and effective transition back to daily activities.