Purpose/Background
Addressing Social Determinants of Health (SDOH) is crucial for improving health outcomes.
Case role-playing scenarios in medical education help students practice in simulated clinical settings, increasing comfort with addressing SDOH routinely.
The study evaluates the impact of case role playing on addressing SDOH in medical education.
It provides practical experiences for students to enhance their navigation of SDOH in patient encounters.
Develop future physicians who instinctively address SDOH in every patient encounter due to early implementation of case role play educational activities.
Methods
Setting: UNTHSC TCOM campus
Participants: Third Year Medical Students in Family Medicine Clerkship
Measures: Pre and Post Surveys, individual reflections, and focus group discussions
Outcomes: Improved knowledge and skills, increase comfort in addressing SDOH, and enhanced understanding of challenges.
Analyses: Quantitative and qualitative analysis of assessments/surveys, reflections, and discussions
Sequence of Activities
First Activity: Pre-Survey
Second Activity: SDOH Didactic Lecture
Third Activity: Case Role Play
Student Evaluator – Student Doctor – Student Checklist Assessor – Student Patient
Fourth Activity: Individual Reflection, Small Group Discussion & Large Group Discussion
Fifth Activity: Post Survey
Sample Script of Activity
47 year old woman presents to your office for an annual physical examination. She reports that she is very healthy and has no specific complaints. Her PMH is significant for seasonal allergies and well controlled mild, intermittent asthma. She is married and has 2 children via normal spontaneous vaginal delivery without complication. She takes a multivitamin daily and antihistamines and a puff of an albuterol inhaler on occasion. Her family history is significant for hypertension and type 2 diabetes mellitus in her father, depression in her mother and sister, and breast cancer diagnosed in her maternal grandmother at age 72. The patient is married and monogamous, gets regular exercise, and does not smoke cigarettes, drink alcohol, or use illicit drugs.
Vitals: Her vitals are blood pressure is 129/79 mmHG, pulse is 74 beats/min and regular, height is 67 inches, weight is 152 pounds, BMI is 23.8kg/m2 and abdominal waist circumference is 32 inches.
Physical Exam: Her physical examination is unremarkable.
Sample of Visit Checklist
1. Screening
☐ Blood pressure
☐ Breast cancer
☐ Cervical cancer
☐ Intimate Partner Violence
☐ Colon Cancer
☐ Hepatitis C
☐ HIV
☐ Social Determinants of Health
☐ Tobacco use
☐ Alcohol use
☐ Drug use
☐ Anxiety
☐ Depression
☐ Cardiovascular risk evaluation – going over vitals; labs HLD evaluation
2. Immunizations
☐ Tdap
☐ Flu
☐ COVID
☐ PCV 20 – Due to history of asthma
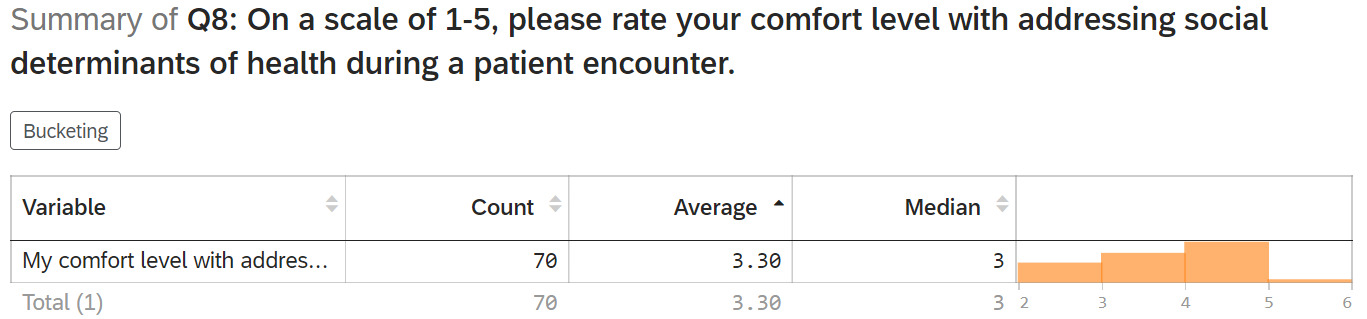
SDOH Pre-Survey
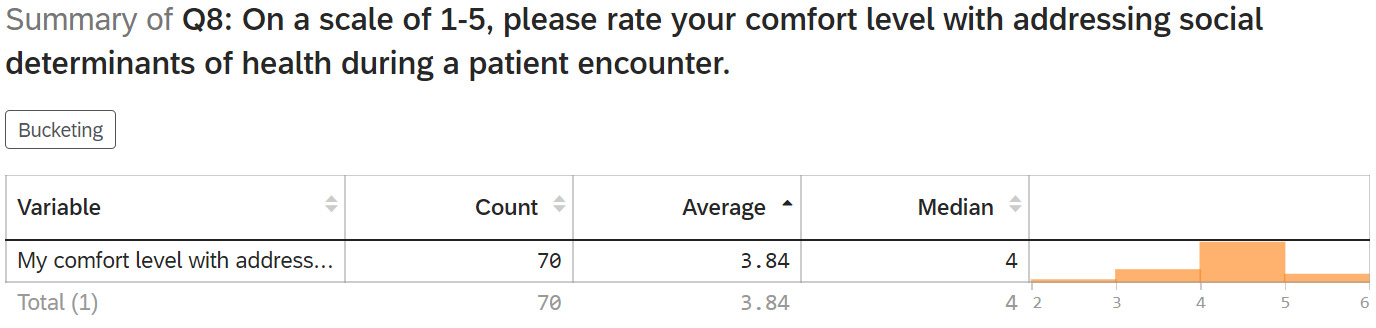
SDOH Post-Survey
P value – 0.0001 Confidence Interval -0.78 to -0.31
What were some challenges you encountered when participating in this activity?
Reflection comments by students
“Hard to bring up social determinants of health and explain in your own words”
“You had to establish trust to get better answers on Social determinants of health”
“The next most challenging was transitioning the conversation to discuss social determinants of health.”
Based on the challenges you provided above, create an action plan.
Reflection comments from students
“Try to work in questions regarding social determinants of health throughout the encounter”
“I will also continue reviewing and become familiar with general resources that are available at the clinic and in the area”
Key Findings
Students found discussing and transitioning to SDOH discussion challenging.
They planned to integrate social determinants questions throughout interactions and review available resources.
Case role play activity increased their comfort in addressing SDOH during patient encounters.
Conclusion
Main Findings and Interpretations
Initial challenges in discussing SDOH highlight the need for case role play interventions.
Post-activity action plans show case role play positively influences clinical practice.
Overall, the activity boosts student comfort in addressing social determinants, enhancing skills and potential better patient outcomes.
Future Implications of Study
Extend case role play to high-yield Family Medicine topics beyond SDOH.
Enhance education for diverse healthcare professionals at all levels of education and foster a patient-centered approach during clinic encounters.
Limitations
Limited generalizability due to single-institution study.
Potential bias in self-reported comfort levels
Case role play scenarios may not fully replicate real-world patient encounters.
Lack of long-term follow-up to assess sustained impact.